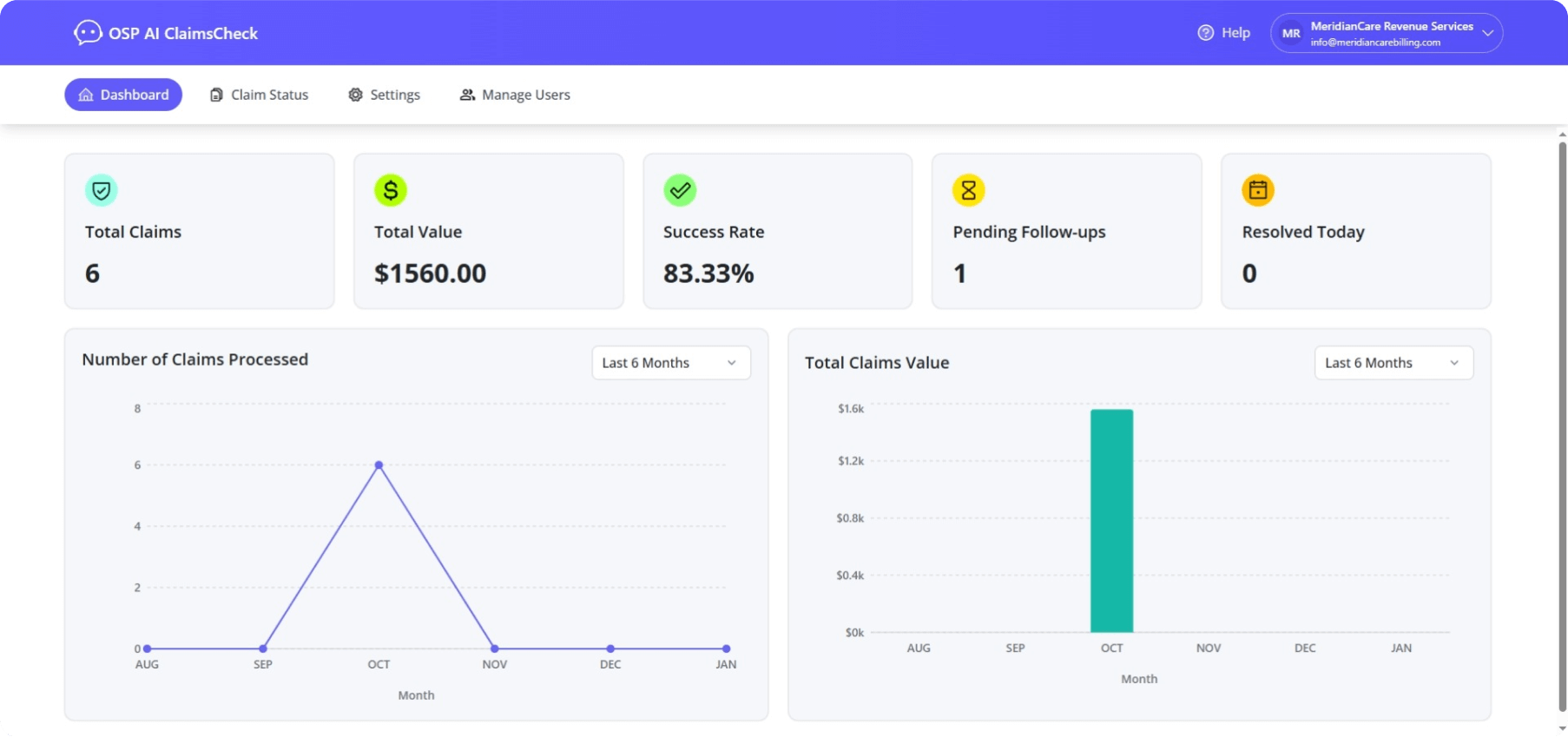
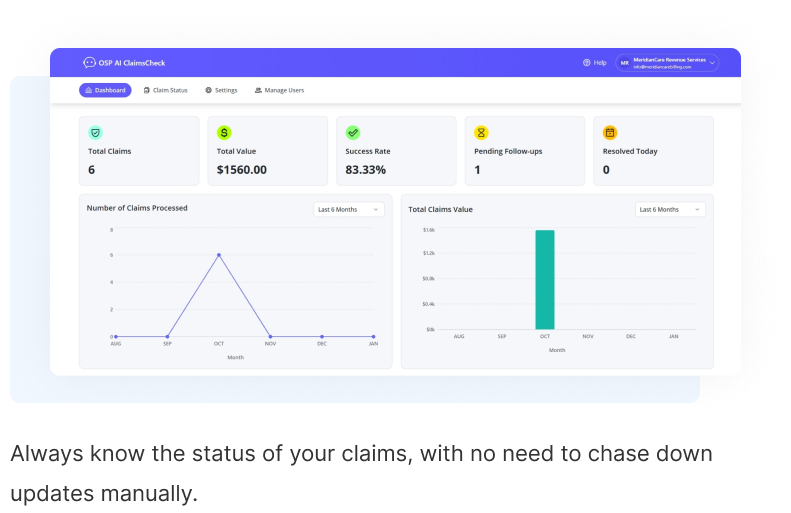
Agentic AI claims platform is your silent partner, reducing hours of manual labor and making your billing process more efficient. Instead of spending precious time on repetitive tasks like payer calls, portal logins, and follow-up emails, your team can focus on increasing client results and driving business growth.
Faster reimbursements and a reduced A/R all while maintaining audit-ready transparency.
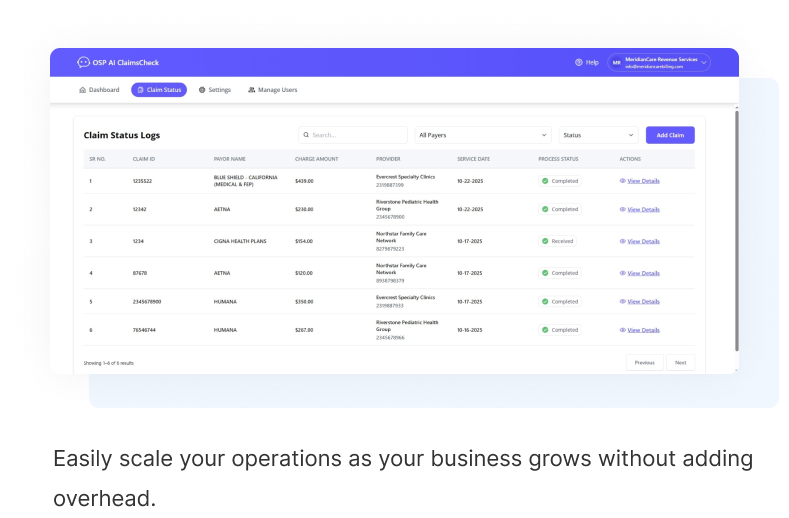
Our agentic AI platform for medical claims management is built for high-volume claims processing. Whether you manage thousands of claims across multiple locations or specialize in specific payer types, our automation can scale with your needs, reducing turnaround times and eliminating manual follow-ups.
Increased efficiency and the ability to manage claims at scale without adding headcount.
Your team's time is valuable. OSP's Agentic AI claims platform helps you focus on patient care rather than endless payer delays. Our AI platform integrates seamlessly into your existing workflow, automating the process of checking claim statuses across phone and payer portals.
ero disruption to daily operations and a smoother, more efficient billing experience for your practice.